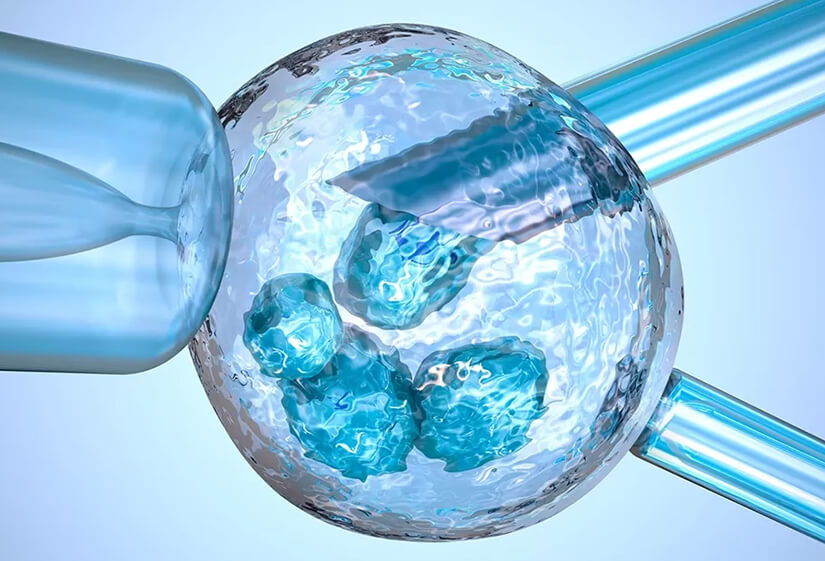
In vitro fertilization (IVF) is a multi-step medical procedure specialists design to assist with conception. IVF involves retrieving eggs from the ovaries, and fertilizing them with sperm in a laboratory. Once embryos form, they are either transferred to a uterus, frozen for later use, or biopsied for genetic testing. Here is more information about the role of genetic testing for this treatment:
Finding Healthy Embryos
Genetic testing of embryos, known as preimplantation genetic testing (PGT-A), is an option available during the IVF process. After the embryos develop for several days in the laboratory, an embryologist performs a biopsy to collect a small sample of cells. The sample comes from the trophectoderm, which is the part of the embryo that will later form the placenta, and specialists perform this process with precision.
They then send the collected cells to a specialized laboratory for genetic analysis. This testing helps identify chromosomal abnormalities, which may affect embryo viability. While PGT-A can improve the chances of selecting a healthy embryo, it does not guarantee a successful pregnancy.
Sending Samples to Labs
They then send the collected cell sample to a specialized genetics laboratory for analysis, and the embryology team freezes the biopsied embryos while awaiting the results. Laboratories use advanced techniques to screen the cells for specific genetic or chromosomal abnormalities. This detailed analysis, which provides genetic information about each embryo, offers valuable insights into their respective genetic profiles.
Making Selections
Once the genetic testing report is received from the lab, they review the results. The report details which embryos are chromosomally normal, which are abnormal, and which may have a mix of normal and abnormal cells. The information is then used to select an embryo for transfer.
Selection is a methodical process. The goal is to identify a euploid embryo so that you can proceed to the next stage. This report guides this selection, but other factors like embryo grading also contribute to the final decision.
They document the final choice before proceeding to the next step. Since the embryos were frozen after the biopsy, they must thaw the selected embryo in preparation for the transfer procedure. This careful process of thawing is timed to align with the recipient’s uterine cycle. The laboratory staff manages this timing carefully, and the clinical team prepares the patient accordingly.
Preparing for Implantation
Preparing the uterus for implantation involves a specific hormonal protocol. The patient will take medications, like estrogen and progesterone, to create a receptive uterine lining for the embryo. While the body prepares, clinic appointments will monitor the lining’s thickness and hormonal levels through ultrasounds and blood tests. Once the uterine lining reaches the optimal thickness and hormonal levels are confirmed, the clinic will schedule the embryo transfer. This careful preparation may increase the likelihood of a successful implantation and subsequent pregnancy.
Schedule IVF Therapy Today
Genetic testing is one component of the broader IVF journey. The process involves multiple stages, from initial stimulation and retrieval to laboratory analysis and eventual transfer. Specialists coordinate each step between the clinical team, the laboratory, and the patient. To learn more about the IVF process and its associated procedures, contact a fertility clinic to schedule a consultation with a specialist.